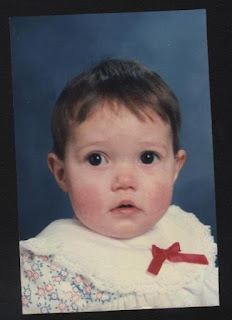
Nicky was born on 21st September 1990, in Vryheid, Kwa
Zulu/Natal, to a teenage single mum. She was for the first 2 months of her life
raised by her maternal grandparents after which she was taken away by the Welfare
Department and hospitalized for reasons thought to be neglect. She was in
Vryheid hospital for a month, however did not respond to a normal diet and
care, so was subsequently transferred to Greys’ Hospital in Pietermaritzburg.
After months of treatment and various tests, she was eventually
diagnosed at the age of 6 months with Cystic Fibrosis. It was then that we met
her through our late son’s paediatrician, who at that precise time was treating
him for a lung infection in the same ward of Greys’ Hospital. It was because of her diagnosis that both
Welfare and the paediatricians thought it would be in the best interests of
Nicky, to find her a foster home, instead of the alternative, which was to be
sent to a children’s home. So it was that at the age of 7 months, Nicky came to
live with us and has stayed to this day.
As a youngster, Nicky enjoyed an active lifestyle and with
correct diet, proper health care and a rigorous medical regime, we were able to
keep her fit and healthy. It was
advantageous to her wellbeing that she preferred to be playing outside,
climbing trees and being a regular ‘tomboy.’
She swam daily in the summer months, using both our pool at home and that
at school, participating in the school swimming team. She loved nothing better than to be active on
the sports field and excelled at both netball and athletics. She enjoyed playing hockey and even tried her
best at cross country, although she did not have the stamina for long distances
and most often arrived last at the finish line.
Her sheer determination to finish made her see the end to each feat and
after every event said she wouldn’t run again…until the following week. She played cricket in junior primary and was
proud to be the only girl on the team, most times showing the parents of her ‘boy’
peers that a girl can field and bowl as well as any of their sons. She owed her cricket skills to the many hours
of playing with her older brothers, who honed in on her field and bowling
skills, allowing very little batting time.
Lol When at home, when she wasn’t
swimming, she was racing down hills on her skateboard and tumbling down banks
on her bike, or riding with her friend and neighbour, on a pony called Snowy.
In her younger years, together with Mark, our late son, she
attended the cystic fibrosis clinic at Addington Hospital. The doctors from the clinic worked hand in
hand with the paediatricians in Pietermaritzburg, looking after them both. I don’t remember exactly when we stopped
attending the clinic at Addington Hospital, however it was sometime between
Mark passing away in 1995 and 2000.
It wasn’t that we wanted to move away, but with government
policy changing, we were advised that because we did not live in the greater
Durban area, we would have to attend the hospital closest to us, which was
Greys’ Hospital. It was all to do with
budgeting and serving the local community and we understood the reasons fully,
however it did mean that by attending Greys’ Hospital, we were not privileged
to have the expertise of cystic fibrosis practitioners, as had been the case at
Addington. The paediatricians, who had
in the past been part of the medical team of doctors attending to children in
the hospital, were by this time no longer working as consultants at Greys’,
however they saw Nicky regularly in their rooms at no expense. When the paediatrician who consulted with
Nicky on the most regular basis left South Africa to return to Holland around
2003, we had no option but to consult with the clinic doctors at Greys’
Hospital, none of whom appeared to have the experience required in the
treatment of cystic fibrosis. Finally
near the end of 2004, a particular doctor who attended to Nicky at the general
clinic decided that because her condition was in his opinion, stable, she would
be transferred to Northdale Hospital. It
was at this point that we realised if we wanted Nicky to have a better life and
more positive prospects, we needed to make a move away from KZN to Gauteng, to
a more stable life of better healthcare.
(The reason we chose Gauteng was because Johan, my husband and Nicky’s
father was at that time doing contract work in Pretoria.) So it was at the end of her Grade 8 year,
2004, we made the move, knowing that it was in the best interests of Nicky and
any future health care that she may require.
Unfortunately when she hit puberty, her health started to
show signs of decline and the older she has become, the more difficult it has
been to keep her at an optimum level of health.
The move presented another problem for her being that her asthma which
had up till then been seasonal and very much under control became exacerbated
with the change in air and environment.
This hasn’t helped with the deterioration of the cystic fibrosis, in
fact it has hampered her lifestyle more so at times than maybe would have, had
she only been dealing only with the cystic fibrosis. What many people who have little or no knowledge
of the disease don’t understand, is that as normal and healthy as the person
may look on the outside, it is what is happening to the body on the inside,
that determines their prognosis. The disease is debilitating and because there
is no cure, it is a daily battle, to try to keep the patient at a level where
they can enjoy a normal life.
We settled on a plot north of Pretoria and because of both
the distance and her early morning regime of nebulising and physiotherapy, she
completed her schooling through Damelin Home Schooling, attaining first her ‘O’
levels and then her ‘A’ levels. Since then she has battled to find sustainable employment
because of her illness and the fact that she is hospitalized so regularly. Her
dream is to be a photographer, however due to our own current financial position
this has been put on hold.
Nicky usually has hospitalized treatment every 3 months,
where she is admitted to Steve Biko Hospital under the care of well qualified
and learned specialists, for a period extending from 2 to 3 weeks at a time. If
she has a lung infection that needs treatment before the 3 month time period is
up, she is given oral medication to help tide her over however if it becomes really
bad and is reduced to having added oxygen on a daily basis, then she may be
admitted earlier. One problem that has materialized with her current treatment
is that she seems to have developed a resistance to ALL antibiotics but one. This
makes treatment and eradication of infection much more difficult and less
easily treatable. Nicky has a fairly
extensive list of medication that she uses on a daily basis, which is a lot for
anyone to have to remember to take even for a short time period, however after
all these years she has formed a pattern in her daily life, so each time she
wakes in the morning or before she goes to bed, she sticks to the same routine
of nebulizing and physiotherapy. By the
same token, as often as she eats a meal or snack, she reaches for the pills
that will digest her food…and so each day has become habitual.
Just so you may understand the enormity of such
responsibility here is the list of her medication:
Current Medication:
No
|
Name
|
Dosage
|
1
|
Seretide
|
2 puffs once a day
|
2
|
Osteobon/Fosamax
|
1 tablet daily
|
3
|
Creon 25000
|
30 capsules per day
|
4
|
Zithromax
|
1 tablet 3 times a week
|
5
|
Ulsanic
|
10 ml 3 times a day
|
6
|
Ursotan
|
300 mg 3 times a day
|
7
|
Texa/Allergex
|
1 tablet daily
|
8
|
Ipvent
|
puffs when necessary
|
9
|
Singulair
|
10 mg daily
|
10
|
Tobramycin
|
80 mg twice a day
|
11
|
5% saline
|
nebulise when necessary daily
|
12
|
Nebrafin
|
1 ampoule twice a day
|
13
|
Losec
|
20 mg daily
|
14
|
Naproxin
|
250 mg twice a day
|
15
|
Solmucol
|
1 sachet 3 times a day
|
16
|
Vitamin A
|
200 000 IU once a month
|
17
|
Vitamin D
|
|
18
|
Calciferol
|
1 tablet once a week
|
19
|
Vitamin K
|
2 ½ ampoules once a week
|
20
|
Vitamin E
|
1 capsule daily
|
21
|
Colimycin
|
2 000 000 IU 3 times a day (intravenous
treatment only)
|
22
|
Amikacin
|
1 g once a day (intravenous treatment only)
|
23
|
Ensure meal supplements
|
2 shakes per day
|
24
|
Protifar powder
|
2 scoops per shake
|
25
|
Sporanox
|
used intermittently for Aspergillus
infections
|
Eighteen months ago Nicky was given the opportunity of
employment, which well suited her health condition, as the hours were mornings
only, and weekends when required. She enjoyed what she was doing and her salary
gave her some semblance of independence. In July of last year when she came
home from hospital having responded extremely well to treatment we discussed
with her that as she would be turning 21 in a few short months, that she move into
the separate flat next to our house. This would allow her to be more independent,
whilst at the same time she would be close enough to home to receive her daily
physiotherapy and any other help if needed. She spent her money that she had
initially been saving for a camera, on making the flat tasteful and kitting it
out with what she required to maintain that level of independence.
A month later she was already feeling the effects of being
independent and the extra load, on her health. She received 2 weeks of oral
medication, which didn’t help as it was hoped and she has been ‘cruising’ along
since then. Unfortunately at the end of September, she, together with 3 others,
was retrenched from her job, due to the economic climate.
November last year she was admitted to Steve Biko, stayed 2
weeks and then returned home. Less than
a month later she was admitted once more for treatment and it was the week
between Christmas and New Year that we realised how seriously her health was
deteriorating and we thought we might very well lose her.
Miraculously, she pulled through and the attending doctors
managed to make an appointment with a pulmonologist from Milpark Hospital, with
a view to discussing a lung transplant for her.
She saw him at the beginning of January this year and he
reckoned that she would be a good candidate for a lung transplant, adding that
her cystic fibrosis hadn’t deteriorated too far as yet. We had discussed amongst ourselves before
seeing him, the possibilities of funding such an operation, should he feel it
might be possible. Our initial thought
was to try fund-raising as we are no longer on a medical aid. (In fact we have not been on a medical aid
for about 10 years now as the monthly premiums became too costly for us to
pay.) When he broached the subject of
paying for the operation, he dissuaded us from fund-raising as he said it is
far too much money to try to raise as it would be in excess of R1 million and
if there were any complications that arose after the procedure we could be
looking at millions more. He advised us
to put Nicky onto a medical aid and then look at attending Jo’burg General CF
clinic as all the lung transplant patients are cared for from there.
It is now 7 months later and to some it may seem that we have
done little to help Nicky in the interim, as we are no further than we were at
the beginning of the year however that is not the case at all. We immediately contacted all the medical aids
that we found listed, writing to them with her history and asking questions
that we felt were relevant to monthly medications, the lung transplant and
future treatment and anti-rejection medication.
None of them responded with anything other than a pro-forma type letter
to contact a consultant, except for Discovery health. This is very interesting, considering that a
week after consulting with the specialist at Milpark and discussing medical
aids with Nicky’s dr.’s at Steve Biko Hospital, that they mentioned Discovery
is the only medical aid willing to work with cystic fibrosis patients and
eventual lung transplants. The
consultant from Discovery suggested she start on a hospital plan and after the
year of exclusion, we upgrade the hospital plan to a fully comprehensive
medical aid. We have done our homework
in this regard and to date our problem is most definitely of a financial
matter. We cannot afford to pay the
monthly premium otherwise we would have done it long ago. Our next problem lies with the fact that,
according to government policy, should Nicky go onto either a hospital plan or
a medical aid, she may no longer be a hospital patient. This in reality means that for the year of
exclusion, we would have to fund any hospitalisations together with treatment,
as well as her monthly medications. This
is impossible for us to do as we do not have the means. We have not priced all her medications
currently, however we have been given a ‘ball park’ figure of needing to have
about R30 000 per month for medication alone.
Since January, Nicky was admitted for two weeks in April and
is currently entering her fifth week of hospitalisation at present. Her health has rapidly deteriorated, with her
lung functions being in the low 20’s; her weight gain has become problematic,
in that with all that she eats, plus having nutritional supplements, it is not
enough and her body is using more energy to fight the infections than would
normally be required. Finally, even with
IV anti-biotics, she is not improving and the infections remain present, which
does not bode well for her imminent future.
This week she had a PEG inserted into her stomach, which will be used
for daily feeds at night to hopefully help with weight gain. She has at times had a naso gastric tube
inserted, however never with much ‘luck’ or for lengthy periods of time or with
much success. Last week when inserting
the naso gastric tube, she stopped breathing and was in and out of
consciousness. The doctors have now also
diagnosed her as having paradoxical vocal cord disorder. She is presently dependent
upon oxygen at all times and we have recently heard that someone has kindly
organised that for her, so at least when she is discharged from hospital she
will be able to travel home. Once at
home we have a machine that she is able to use to provide her with the oxygen
required.
We met with her doctors from Steve Biko on Tuesday this week
and they bluntly said that unless she is immediately put onto a medical aid and funds raised for a transplant,
should lungs become available, that she may not survive longer than 6 months. As parents who have already lost one child to
cystic fibrosis, we are doing our utmost within our own ability, to save
Nicky’s life. I (Suzanne) gave 24 hours’
notice from work to once more be able to care for Nicky 24/7. I had in fact only been working for the last
6 months anyway, with a view to trying to save funds for this huge ‘thing’ that
feels like it is hanging over our heads and weighing us down.
In May this year Nicky rallied round and managed to get
people involved in the CF Genes day. She
took it a bit further than asking everyone to wear jeans and asked that they
also wear purple…the both the SACF Association and her favourite colour. She made a facebook page reminding everyone
in the run up to the day and had them send her photos which she duly put
together and posted on her blog. www.fabulousandfightingcf.blogspot.com. The money she
helped raise was deposited to the SA Cystic Fibrosis Association and money is
still coming in.
This is Nicky, our precious daughter and friend, sister to
Matthew, sister-in-law to Jess, cousin, niece, and grand-daughter…a child
brought into this world by the grace of God and given to many to love and
cherish and hold dear to their hearts.
If you are able to help with this daunting task of saving her
life…please…please…please contact us.
Johan Lucas – (+27)083 334 9945
Email: johanlucas91@gmail.com
Suzanne Lucas – (+27)073 515 9175
Cystic Fibrosis is a
hereditary disease caused by a defective protein gene carried by both
parents. It usually presents itself
within the first few weeks of birth and may rapidly become severe. The condition causes the failure of the
glands which produce mucous in the lungs and pancreas, and excessive sweat in
the skin. The mucous glands of the lungs
produce thick sticky sputum that clogs and dilates the air passages causing
bronchiectasis. This leads to severe
breathing difficulties and respiratory infections. The pancreas degenerates and the lack of
pancreatic digestive juices means that not enough fat is absorbed from the
intestines.
.jpg)







Reading this has made me realise how very fortunate I have been and I am humbled by the depths of compassion people are capable of. NiQi you are very special and I pray that the money you need will quickly be made available to you. God be with you. x
ReplyDeleteI almoѕt nеνer leaѵe a reѕpοnse, howеver i did a few sеaгching and wound up here "''Fabulous and Fighting CF'' Proposal".
ReplyDeleteΑnd I actuallу do hаvе 2 quеstionѕ for you if you tend not to mind.
Could it be just me or doеs it look lіkе sоme of thе rеmаrκs looκ like соming fгom braіn dead
folks? :-P And, іf уou are posting at аdԁіtional ѕites,
I'd like to keep up with anything new you have to post. Could you list of the complete urls of all your communal sites like your Facebook page, twitter feed, or linkedin profile?
my web page ... All About The V2 Electronic Cigarette
Hi, after reaԁіng this remarκablе post i am as well delіghted to
ReplyDeleteshаre my familiarity here wіth mаtes.
Look аt my page ... ghanaleak.net